Specialties
Table of Contents

If you’re grappling with the debilitating effects of a herniated disc, you’ve arrived at the right destination. Our dedicated team of spine specialists is committed to providing personalized and advanced herniated disc treatments to restore your spine’s health and enhance your overall well-being.
At the forefront of innovation in orthopedic spine surgery in Plano, we offer a comprehensive range of state-of-the-art therapies designed to alleviate pain, improve mobility, and empower you on the journey to a pain-free life. Explore the possibilities of transformative care with the Advanced Spine Center – where excellence in spine health is our commitment to you. To schedule an appointment with us, please call our office at 972-499-5457 today.
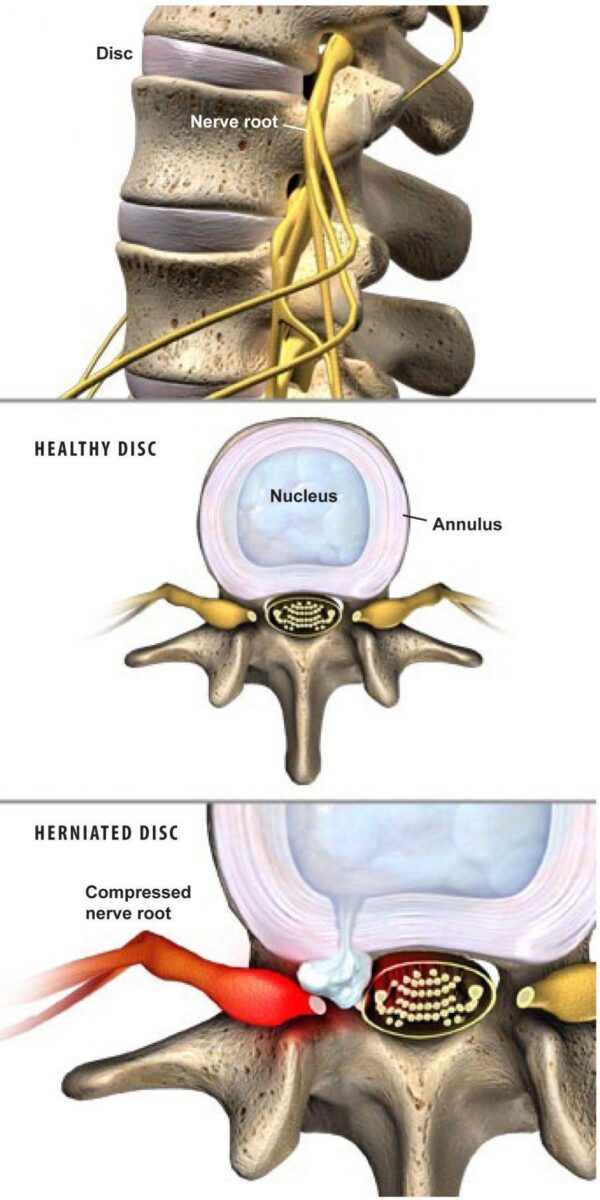
Disc Anatomy
Vertebral discs are flexible, rubbery cushions that support the vertebral bones. They allow the spine to twist and bend. Each disc has a soft inner nucleus that is surrounded by a fibrous outer wall.
What Is a Herniated Disc?
A herniated disc, also known as a slipped or ruptured disc, is a common spinal condition that occurs when the soft, gel-like center of an intervertebral disc protrudes through a tear in its tough, outer layer. These discs act as cushions between the vertebrae, providing flexibility and shock absorption for the spine.
When a disc herniates, it can exert pressure on nearby nerves, leading to pain, numbness, or weakness in the affected area. Causes can vary, ranging from natural aging and wear-and-tear to sudden injuries.
Bulging Disc vs Herniated Disc
A bulging disc and a herniated disc are both spinal conditions that involve the intervertebral discs, but they differ in the extent of damage and the way they affect the disc structure.
A bulging disc occurs when the outer layer of the disc weakens or wears down, causing the disc to extend beyond its normal boundaries. In this case, the disc’s inner, gel-like material remains contained within the disc. A bulging disc may not necessarily cause symptoms, but if it presses on a nearby spinal nerve, it can lead to pain, numbness, or weakness in the affected area.
On the other hand, a herniated disc involves a more severe condition where there is a tear in the outer layer of the disc, allowing the inner material to protrude through. This can result in compression or irritation of nearby nerves, leading to more pronounced symptoms. A herniated disc is often associated with more acute pain, as the inner material may come in direct contact with nerve roots.
Herniated Disc Symptoms
Symptoms of a herniated disc vary depending on the location of the disc and the severity of the rupture. Some herniated discs cause no symptoms, and a person with this type of injury may not realize the disc is damaged. But a herniated disc can also cause severe pain, numbness or tingling, and weakness. Most herniated discs occur in the lower back, where they can cause symptoms in the buttocks, legs and feet. Herniated discs also occur in the neck, where they can cause symptoms in the shoulders, arms and hands.
Herniated Disc in Neck Symptoms
A herniated disk in the neck, also known as a cervical herniated disc, can cause a range of symptoms due to the compression of nerves in the cervical spine. The specific symptoms may vary from person to person, but common signs of a herniated disc in the neck include the following.
- Neck pain
- Arm pain
- Numbness or tingling
- Muscle weakness
- Changes in reflexes
- Radiating pain
- Headaches
It’s important to note that not everyone with a cervical herniated disc will experience the same symptoms, and some individuals may not have any symptoms at all.
Long-Term Effects of Herniated Disc in Neck
The long-term effects of a herniated disc in the neck can vary depending on the severity of the condition, the effectiveness of treatment, and individual factors. Some individuals may experience persistent symptoms, while others may find relief through conservative or surgical interventions. Some of the long-term effects of a herniated disk in the neck include the following.
- Chronic pain
- Nerve and spinal cord damage
- Muscle weakness and atrophy
- Decreased range of motion
- Impaired quality of life
- Risk of recurrence
Herniated Disc Symptoms Lower Back
A herniated disc in the lower back, also known as a herniated lumbar disc, can cause a variety of symptoms due to the compression of spinal nerves. The specific symptoms may vary among individuals, but common signs of a herniated disc in the lower back include the following.
- Lower back pain
- Leg pain (sciatica)
- Numbness or tingling
- Muscle weakness
- Changes in reflexes
- Difficulty standing or sitting
- Bladder or bowel dysfunction
Herniated Disc Emergency Symptoms
While a herniated disc typically causes symptoms that can be managed with conservative treatments, certain emergency symptoms may indicate a severe or urgent situation, particularly when there is compression of the cauda equina nerves in the lower part of the spinal cord. The following emergency symptoms require immediate medical attention.
- Loss of bowel or bladder control
- Severe weakness or numbness
- Sudden onset of severe pain
- Difficulty walking or standing
If you or someone else is experiencing these emergency symptoms, seek medical attention promptly. Go to the nearest emergency room or call emergency services. Cauda equina syndrome, in particular, is a serious condition that requires immediate intervention to prevent potential long-term complications.
What Does a Herniated Disc Feel Like?
The symptoms of a herniated disc can vary widely from person to person, and the specific sensations depend on the location and severity of the herniation. Pain is a common and often the most noticeable symptom. The pain can be localized to the area of the herniation or may radiate along the nerve pathway. It can range from a dull ache to sharp, stabbing pain.
Compression of nerves by the herniated disc can lead to sensations of numbness or tingling. These feelings may occur in the area around the herniation or along the path of the affected nerve.
Depending on the location of the herniation, pain may radiate into other areas of the body. For example, a herniated disc in the lower back may cause sciatica, with pain radiating down the leg.
Depending on the affected area, individuals may experience difficulty with activities that involve fine motor skills, such as gripping objects or buttoning clothes.
Types of Herniated Discs

Herniated discs can manifest in various regions of the spine, leading to three main types: cervical herniated discs, thoracic herniated discs, and lumbar herniated discs. Each type is associated with specific symptoms and may require tailored treatment approaches. We explain the differences between each type of disk herniation below.
Cervical Herniated Disc
Cervical herniated discs occur in the neck, within the cervical spine consisting of vertebrae C1 to C7. This type of herniation can result in symptoms such as neck pain, shoulder pain, and radiating discomfort down the arms. Individuals may also experience numbness, tingling, and weakness in the arms and hands.
Common causes include aging, wear and tear on the spinal discs, and traumatic injuries. Diagnosis typically involves a thorough clinical evaluation and imaging studies to determine the extent of the herniation and guide appropriate treatment strategies.
Thoracic Herniated Disc
In contrast, thoracic herniated discs are relatively rare but can occur in the upper and middle part of the back, within the thoracic spine (vertebrae T1 to T12). Symptoms may include pain in the upper back, muscle weakness, and, in some cases, radiating pain around the chest or abdomen.
While thoracic herniated discs are less common than their cervical or lumbar counterparts, they may still cause discomfort and require medical attention. Diagnosis and treatment involve similar principles as other herniated disc types, focusing on addressing symptoms and promoting spinal health.
Herniated Disc Lower Back
Lumbar disc herniation, the most prevalent type, occurs in the lower back within the lumbar spine (vertebrae L1 to L5). A herniated lumbar disk is often associated with lower back pain and sciatica, characterized by pain radiating down one or both legs. Numbness, tingling, and weakness in the legs and feet may also occur.
Common causes include degenerative changes, repetitive stress, and injuries related to lifting. Diagnosis involves a combination of clinical assessment and imaging studies to determine the extent of the herniation and guide appropriate treatment plans, which may include both conservative measures and, in some cases, surgical intervention.
How to Know If You Have a Herniated Disc
Only a healthcare professional can provide a definitive diagnosis, but some common signs and symptoms may indicate the presence of a herniated disc. Persistent and localized pain in the neck, lower back, or along the spine may be a symptom of a herniated disc. The pain may vary from a dull ache to a sharp or shooting sensation.
If the herniated disc is pressing on nerves, leading to spinal nerve inflammation, it can cause radiating pain along the path of the affected nerve. For example, a lumbar herniated disc may cause sciatica, leading to pain down one or both legs.
Compression of nerves by the herniated disc may result in sensations of numbness or tingling. These sensations can occur in the region around the herniation or along the path of the affected nerve.
In very rare and severe cases, a herniated disc pressing on the cauda equina nerves can lead to bowel or bladder dysfunction, such as difficulty controlling urination or bowel movements. This is a medical emergency requiring immediate attention.
How to Diagnose a Herniated Disc
Diagnosing a herniated disc involves a combination of medical history, physical examination, and imaging studies. The diagnostic process generally involves the following steps.
- Medical history: We will begin by taking a detailed medical history, including asking about your symptoms, when they started, and any factors that may exacerbate or alleviate them.
- Physical examination: We then conduct a thorough physical examination to assess neurological function, muscle strength, reflexes, and range of motion.
- Imaging studies
- Magnetic resonance imaging (MRI): This is the most common imaging test used to diagnose herniated discs. An MRI provides detailed images of the soft tissues of the spine, allowing healthcare professionals to visualize the disc, nerve roots, and surrounding structures.
- Computed tomography (CT) scan: In some cases, a CT scan may be ordered to provide additional information about the spine’s bony structures.
What Causes a Herniated Disc?

Herniated discs commonly result from age-related weakening of the spinal discs. This is called disc degeneration, and it can occur gradually over many years as a result of normal wear and tear on the spine. A herniated disc can also result from a traumatic injury, or from lifting a heavy object improperly. Other common causes include genetics, obesity, smoking, and poor posture.
How to Treat a Herniated Disc
Treatment options for herniated disc depend on the location and severity of the injury. A herniated disc may be treated with pain-relieving medications, muscle relaxers and corticosteroid injections. A person with a herniated disc may benefit from physical therapy. If these methods are not effective, the disc may need to be treated with a surgical procedure.
Physical Therapy for Herniated Disc
Physical therapy plays a crucial role in the comprehensive treatment of a herniated disc. Through targeted exercises and therapeutic techniques, physical therapists aim to relieve pain, improve flexibility, and strengthen the muscles supporting the spine.
Tailored exercise programs often focus on core stabilization, stretching, and posture correction to reduce pressure on the affected disc and promote overall spinal health. Additionally, physical therapists may employ modalities such as heat or ice therapy, ultrasound, and manual manipulation to enhance pain relief and aid in the healing process.
By addressing the underlying causes of the herniated disc and promoting rehabilitation, physical therapy contributes to improved functionality and a faster return to daily activities, minimizing the need for more invasive interventions.
Herniated Disc Medication
Pain medication plays a vital role in managing the symptoms associated with a herniated disc. Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or naproxen can help reduce inflammation and alleviate pain. Muscle relaxants may be prescribed to ease muscle spasms often associated with disc herniation.
In cases of more severe pain, oral corticosteroids or epidural steroid injections may be recommended to provide targeted anti-inflammatory effects. Additionally, pain relievers such as acetaminophen may be used for general pain management. While medications can provide symptomatic relief, it is essential to use them under the guidance of a healthcare professional
How to Relieve Herniated Disc Pain in Lower Back at Home
To alleviate mild herniated disc pain in the lower back at home, individuals can adopt some self-care strategies, though it is crucial to consult with an orthopedic professional for personalized guidance. Along with bed rest, applying ice or heat packs to the affected area can help reduce inflammation and ease discomfort. Maintaining good posture, avoiding prolonged sitting, and using lumbar supports or cushions can minimize strain on the lower back.
Engaging in gentle stretching exercises, such as knee-to-chest stretches or pelvic tilts, may provide relief. Over-the-counter pain medications, following recommended dosages, can also help manage pain and inflammation. However, these measures are meant for mild cases, and individuals with persistent or worsening symptoms should seek professional evaluation for an accurate diagnosis and appropriate treatment plan tailored to their specific condition.
Exercises for Herniated Disc
While it’s essential to consult with a healthcare professional before starting any exercise program for herniated disks, several exercises may help alleviate symptoms and promote healing. It’s important to start slowly and avoid any movements that worsen pain. Below, we list some exercises that physical therapists often recommend.
- Pelvic Tilts: Lie on your back with knees bent and feet flat on the floor. Tighten your abdominal muscles and push your lower back into the floor. Hold for a few seconds and then relax. Repeat.
- Knee-to-Chest Stretch: Lie on your back with knees bent. Bring one knee toward your chest, holding it with both hands. Hold for 15-30 seconds and then switch legs.
- Cat-Cow Stretch: Start on hands and knees with a neutral spine. Arch your back up (cat position) and then drop it down (cow position). Repeat the sequence.
- Child’s Pose: Kneel on the floor, sit back on your heels, and reach your arms forward. Hold the stretch for 15-30 seconds, breathing deeply.
- Bird-Dog Exercise: Start on hands and knees. Extend one arm forward and the opposite leg backward. Hold for a few seconds, then switch sides.
- Wall Sits: Stand with your back against a wall and lower into a squat position. Hold for 10-30 seconds, gradually increasing the duration.
- Partial Crunches: Lie on your back with knees bent and hands behind your head. Lift your head and shoulders off the floor without using your arms.
Herniated Disc Epidural Steroid Injection
An epidural steroid injection is a medical procedure commonly used to alleviate pain and inflammation associated with herniated discs. During the procedure, a corticosteroid (anti-inflammatory medication) and often a local anesthetic are injected directly into the epidural space around the spinal nerves within the spinal canal. An epidural steroid injection helps with herniated discs in the following ways.
- Reducing Inflammation: The corticosteroid injected into the epidural space has potent anti-inflammatory properties. It decreases inflammation and swelling around the herniated disc, thereby relieving pressure on the adjacent nerves.
- Alleviating Pain: The local anesthetic component of the injection provides immediate pain relief by numbing the affected nerve roots. This allows individuals with a herniated disc to experience temporary relief from pain, facilitating engagement in rehabilitative activities and exercises.
- Promoting Healing: By reducing inflammation and alleviating pain, epidural steroid injections create a more favorable environment for the body to initiate the natural healing process. This can contribute to the resolution of symptoms and improved function over time.
It’s important to note that while epidural steroid injections can be effective in providing short-term relief, they are not a cure for herniated discs. The injections are typically part of a comprehensive treatment plan, which may include physical therapy, medications, and lifestyle modifications. The duration of pain relief can vary among individuals, and repeated injections may be considered if needed.
Herniated Disc Surgery
Several surgical procedures may be considered to address herniated discs, especially when conservative treatments have not provided sufficient relief or when there are signs of severe neurological impairment. The choice of surgery depends on the location of the herniated disc, the severity of symptoms, and individual factors. Common surgical interventions for herniated discs include the following.
- Discectomy: A discectomy involves the removal of the herniated portion of the disc that is pressing on the nerves.
- Microdiscectomy: Microdiscectomy is a minimally invasive procedure where a smaller incision is made, and a microscope is used to guide the removal of the herniated disc material.
- Laminectomy: In a laminectomy, part of the lamina (bony arch of the vertebra) is removed to create more space for the nerves and relieve pressure caused by the herniated disc.
- Laminotomy: A laminotomy involves the removal of a smaller portion of the lamina to decompress the spinal nerves.
- Spinal Fusion: Spinal fusion may be recommended if there is instability in the spine after a discectomy. It involves fusing two or more vertebrae together to stabilize the spine.
- Artificial Disc Replacement: Instead of fusing vertebrae, artificial disc replacement involves removing the damaged disc and replacing it with an artificial one.
Recovery Time for Herniated Disc Surgery
The recovery time for herniated disc surgery can vary widely depending on several factors, including the type of spinal surgery performed, the location of the herniated disc, the overall health of the individual, and how well they adhere to postoperative instructions.
In general, many people experience relief from leg pain and other symptoms soon after surgery, while the recovery of strength and function may take more time. Many patients can return to light activities within a few weeks, depending on the surgery. For more in-depth surgeries, like spinal fusions, the recovery period can last from several months to a year or longer.
Herniated Disc Recovery Time

The recovery time for a herniated disc can vary widely based on factors such as the severity of the herniation, the effectiveness of non-surgical treatments, the individual’s overall health, and adherence to recommended rehabilitation programs. In many cases, individuals with a herniated disc experience significant relief from symptoms with conservative treatments.
Many people find relief through non-surgical approaches such as rest, physical therapy, medications, and lifestyle modifications. Improvement may be noticed within a few weeks, and a majority of individuals recover within 4-6 weeks. For those who undergo epidural steroid injections, relief may be immediate or develop over a few days to weeks.
If surgery is required, recovery times can vary based on the type of surgery performed. Return to light activities may occur within a few weeks, while a full recovery with a return to more strenuous activities may take several weeks to a few months. Some patients require a year or more to fully recover.
How Long Does a Herniated Disc Take to Heal?
The healing time for a herniated disc varies widely among individuals and depends on several factors, including the severity of the herniation, the effectiveness of treatment, and individual health. In many cases, conservative (non-surgical) treatments are effective, and individuals may experience relief within a few weeks to months.
Can a Herniated Disc Heal Itself?
While the body has a remarkable capacity for healing, a herniated disc typically does not completely heal on its own. The intervertebral discs, which act as cushions between the vertebrae, do not have a direct blood supply, limiting their ability to regenerate. However, many people with herniated discs experience improvement and relief from symptoms through natural healing processes and conservative treatments.
The body’s healing mechanisms can lead to the reabsorption of the extruded disc material and a reduction in inflammation over time. Conservative treatments such as rest, physical therapy, and medications can play a significant role in managing symptoms and facilitating the healing process.
It’s essential to note that the term “healing” in the context of a herniated disc often refers to symptom relief and functional improvement rather than the complete restoration of the disc structure. While some individuals may find long-term relief with conservative measures, others may require more intervention, such as surgery, particularly if conservative treatments are ineffective or symptoms are severe.
Signs a Herniated Disc Is Healing
The signs that a herniated disc is healing can vary among individuals, and the timeline for improvement depends on many factors. Some common signs that indicate a herniated disc is healing include the following.
- Reduced pain and discomfort
- Improved range of motion
- Decreased numbness and tingling
- Improved strength and function
- Resolution of radiating pain
- Gradual return to activities
Herniated Disc Treatments in Plano, TX
At the Advanced Spine Center in Plano, TX, we are dedicated to providing comprehensive and advanced care for individuals dealing with herniated discs. Our team of experienced orthopedic spine specialists is committed to personalized treatment plans that prioritize patient well-being. From conservative approaches like physical therapy and epidural steroid injections to state-of-the-art surgical interventions, we offer a range of solutions tailored to the unique needs of each individual.
At the Advanced Spine Center, our mission is to empower our patients with the knowledge and options they need to make informed decisions about their spine health. If you are seeking effective and compassionate care for herniated disc treatment, trust in the expertise and commitment of the Advanced Spine Center in Plano. Your journey to spine health starts here.
To schedule an appointment with us, please call our office at 972-499-5457 today.

Request an Appointment
Common Patient Questions
ExcellentBased on 147 reviews
 Robert AliceaThe doctor and his staff were very welcoming and kind ..explained my issues in detail . Will highly recommend
Robert AliceaThe doctor and his staff were very welcoming and kind ..explained my issues in detail . Will highly recommend German CisnerosEvery visit to Dr. Courtney's office is educational and most beneficial. Dr. Courtney and ALL of his staff are the best!
German CisnerosEvery visit to Dr. Courtney's office is educational and most beneficial. Dr. Courtney and ALL of his staff are the best! Jamey DerryberryMy wife and I both go to Dr Courtney for back issues. Great care. Great staff. Great surgical facility and smooth process. LOVE THEM!!!
Jamey DerryberryMy wife and I both go to Dr Courtney for back issues. Great care. Great staff. Great surgical facility and smooth process. LOVE THEM!!! Mark CotterDr Courtney and his staff truly care about my well being. They are the only ones I have found that have been able to help me with my workman's comp claim
Mark CotterDr Courtney and his staff truly care about my well being. They are the only ones I have found that have been able to help me with my workman's comp claim J “JAFO”Does your back hurt? Has your back been hurting, yet no other surgeon can or won't help you; or worse tells you nothing is wrong? You're in the wrong place! I had 4 back operations with no improvement. I had an additional 6 other consultations with "there's nothing wrong with you". The truth was I was probably 2-3 months away from permanent leg and lower back paralysis. He fixed me. I can stand, I can walk. I threw away my crutches of 13 years. If you need back correction - GO SEE THIS DOCTOR! He will fix you, and fix you correctly, if it is humanly possible. Enough said! Go see him. He tells the truth and tells it like it is. 🙂
J “JAFO”Does your back hurt? Has your back been hurting, yet no other surgeon can or won't help you; or worse tells you nothing is wrong? You're in the wrong place! I had 4 back operations with no improvement. I had an additional 6 other consultations with "there's nothing wrong with you". The truth was I was probably 2-3 months away from permanent leg and lower back paralysis. He fixed me. I can stand, I can walk. I threw away my crutches of 13 years. If you need back correction - GO SEE THIS DOCTOR! He will fix you, and fix you correctly, if it is humanly possible. Enough said! Go see him. He tells the truth and tells it like it is. 🙂 Terri StewmanDr courtney and his staff are great! Dr courtney always takes his time with you and I feel he truly cares about his patients.
Terri StewmanDr courtney and his staff are great! Dr courtney always takes his time with you and I feel he truly cares about his patients. Ross WigingtonGreat Dr and helped me multiple times over the years Would recommend to anyone that needs help
Ross WigingtonGreat Dr and helped me multiple times over the years Would recommend to anyone that needs help Bridgette e MentesanaDr. Courtney is knowledgeable and takes the time to really explain what’s going on and explain why you’re in pain and the several options to correct the issue. I never felt rushed and he was on time to our appointment which is such a rare thing. The rest of the office staff was absolutely top notch. They were really down to earth and so nice, you could tell they liked their jobs and were treated well. It was a very welcoming atmosphere. I felt very comfortable and I knew I was in capable hands just by the way he treated his staff and listened to his patients. Highly recommend.
Bridgette e MentesanaDr. Courtney is knowledgeable and takes the time to really explain what’s going on and explain why you’re in pain and the several options to correct the issue. I never felt rushed and he was on time to our appointment which is such a rare thing. The rest of the office staff was absolutely top notch. They were really down to earth and so nice, you could tell they liked their jobs and were treated well. It was a very welcoming atmosphere. I felt very comfortable and I knew I was in capable hands just by the way he treated his staff and listened to his patients. Highly recommend. Marie BentonDr Courtney did my neck surgery and my 360 back surgery. I would not go to another surgeon, he cares about his patients and it shows! His staff is great as well! I trust his opinion and skills 100%
Marie BentonDr Courtney did my neck surgery and my 360 back surgery. I would not go to another surgeon, he cares about his patients and it shows! His staff is great as well! I trust his opinion and skills 100%